What We Are Fighting For
It has been said, “Poverty is Isolation.” That is especially true in many parts in Kenya.
Places like Kilifi face real hardships.
For example, while Kilifi County has 73 health clinics, a full 57% of the population lives over 3 miles away from their closest clinic.
More alarmingly, for the 720,000 people in the district, there are only 11 practicing doctors. This means that thousands live in great peril if they get sick.
But cell phones break that isolation.
Mobile phones are a routine part of our lives but they are nothing less than a revolution in the developing world. According to the United Nations, there are nearly 5 billion cell phones in the world. Of that, 71% are in the developing world. In Kenya, cell phone coverage is particularly high at 90% of the population. All of a sudden, it is possible to communicate with people in every corner of the globe.
That is where Kilifi Kids comes in.
Our solution: Don’t bring the kids to the clinic—bring the clinic to the kids. We’re going to be taking the medical care to the mothers and children who need it most. Our efforts will be through the cell phone and leverages the existing mobile network–providing a new and cost-effective avenue to provide health to the rural poor.
What We Do
Our work focuses on fixing one of the most broken areas in the care spectrum–the connection between clinicians and patients. The community health worker (CHW) is the secret ingredient in all of this and really brings our mHealth program to life.
A CHW is typically a women chosen from her village and tasked to oversee the health of 10-25 households (150-250 persons) in her community. She serves as the eyes and ears for a health clinic and may receive 2 weeks of basic health training.
The vast majority of CHWs are volunteers in Kenya. As can be imagined, most struggle to make it work: they lack the time; the distance in-between households is too far; and they can’t afford to go unpaid.
Kilifi Kids steps in here and makes it easier for CHWs to do their job, generate a small income, and be change agents in their community. Leveraging Kenya’s established cellular phone network, we put cell phones in CHW hands and provide training on how to use text messages to track patients and then share that data with local health facilities.
Concurrently, we educate the Ministry on how to collect and analyze the health information provided from the field in order to ultimately improve their resource management, streamline clinical workflows, and build a more comprehensive reporting system.
In short, our work provides CHWs with a more direct link to the health system and how to manage patients and follow-up care in the community. Equipped with their mobile phone and a solar charger, CHWs can register every pregnancy and infant in their community, report danger signs to clinical teams, refer sick patients to medical facilities, and coordinate expecting mothers to deliver their babies by a skilled birth attendant.
Our mobile system automates scheduled reminders about future visits: once a CHW receives a notification of an upcoming appointment for a patient, they now make a home visit to encourage a visit to the health facility.
At the same time, the nurse at the health facility now has a more robust system to assess the health status of all patients and ensure a more engaged workforce with better communication.

Where We Work
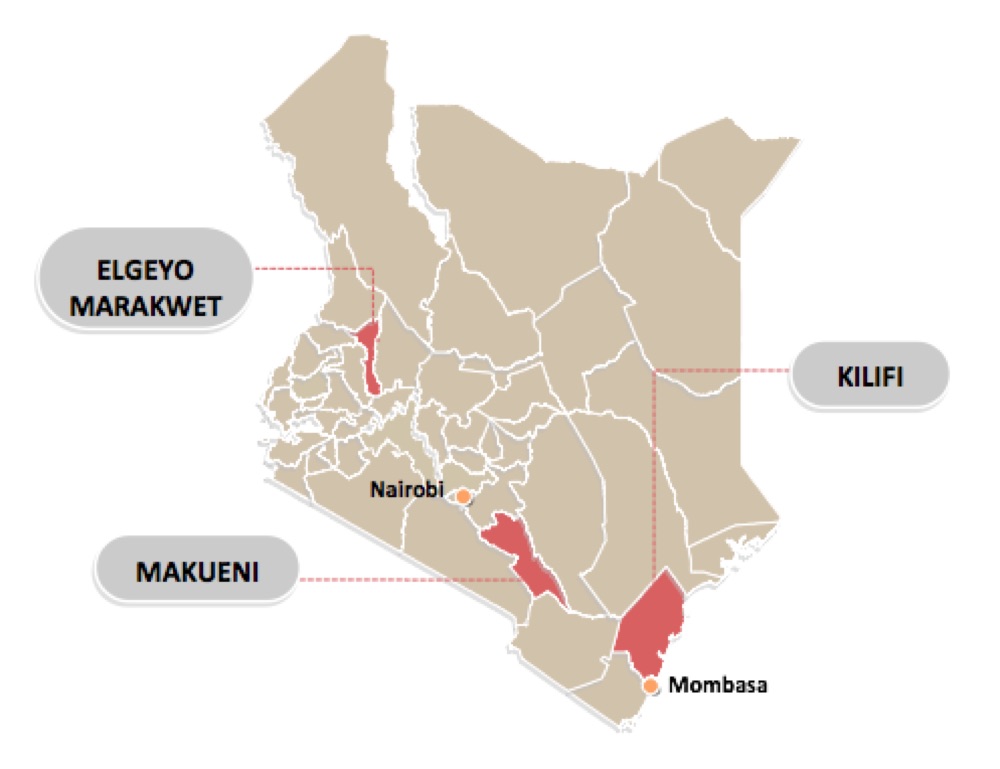
Our work spans coastal, central, and western Kenya across some of the more populated counties in Kenya.
We launched in Kilifi County in 2007 and expanded to Makueni County in 2013. In 2018, after 2 years of planning, we are launching our largest site yet in Elgeyo-Marakwet County. Our ambitions are much larger and we are constantly looking at more places in Kenya and other countries in Africa.
What We Have Accomplished
In the few years since we have launched our work, we have begun to see the signs of community transformations. After this next intervention, we will have trained over 1,000 community health workers across three districts in Kenya, covering more than 100,000 lives in their regions.
Our impact in these areas has already been tangible, not only in realizing a real uptake of health services but also the improvement of patient outcomes. While measurements are still underway and more formal studies are planned, some examples of the headway we have made for mothers and children in certain areas include:
-
33.5% increase in outpatient services over a 2-year period from baseline results
-
10-20% increase in antenatal care where pregnant mothers visiting clinics prior to childbirth
-
Up to an 85% increase in complete immunization for children under five years
-
30% increase in women delivering at a health facility
Our work is also making an economic impact and driving down the costs of care at our sites. Local ministries are realizing significant savings for medical record keeping, fuel costs, and staff time with our solutions.
Additionally, we have setup income-generating activities among our trained community workers to incentive their continual participation in our work. For example, we launched a solar panel program where CHWs rent their panels to neighbors who charge their own phones. In other cases, we created self-run medical kiosks where profits were shared among community members and re-invested into the program.
Our largest measure of success though is our ability to ensure our goodwork continues after our departure. We continue to make real progress here and have made multiple agreements that transfer total project oversight to local Ministries.
The Ministries can now be true owners in our shared work and expand it to help so many more.
A Successful Track Record
While our focus today is on strengthening the connection between community workers and clinicians, we are proud of the successes we have had in the past. Read about three ways we touched lives in our early days and made a difference.
Fighting Terrible Diseases
Students cannot learn when they are sick and underfed. In some places of Kilifi District, it was estimated that infection rates run as high as 85-90 percent. However, there are very safe, inexpensive, and easy-to-administer treatments for some of the main causes of illness in the region, including 4-cent deworming pills that combat parasites affecting most of the school-aged population. Following World Health Organization guidelines, we partnered with Ministry of Health to launch a major 7-year deworming campaign in the Ganze and Vitengeni regions. The intervention proved incredibly successful for 60,000+ and dropped infection rates from 32% to nearly 0%.


A Dream of Education
Only 10% of students go beyond an 8th grade education in Kilifi. While primary education is free, secondary education is not in Kenya. We were pained to learn this and partnered with great local non-profits, KESHO and Moving the Goalposts, to create scholarships to cover high school, including tuition, uniforms, and books. Over a 7-year period, we screened, sponsored, and mentored 33 of the most gifted students who could not afford the high costs of secondary school (about $250 per year for 4 years). [Meet Georgina, a past student writing about her school day.] Participants were profoundly impacted by the experience, where 75% earned top grades in high school and many later pursued higher education.
Bridging The Digital Divide
Having a community fluent in technology is seen as a foregone conclusion in today’s world of computers and SMART phones. This is not the case for many in the world, particularly in 2007 for those in coastal Kenya. We sought to bridge this divide and provided three schools and the Kilifi District Library with computer labs. Along with the equipment, we have worked with Computers for Schools Kenya to educate teachers on how to incorporate computers into the curriculum to improve student education. About 4,000 people received access to a computer and 700 per year have the opportunity to graduate high school being computer literate.

